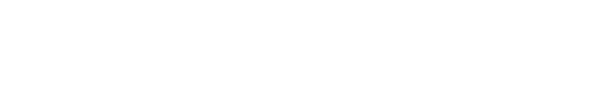
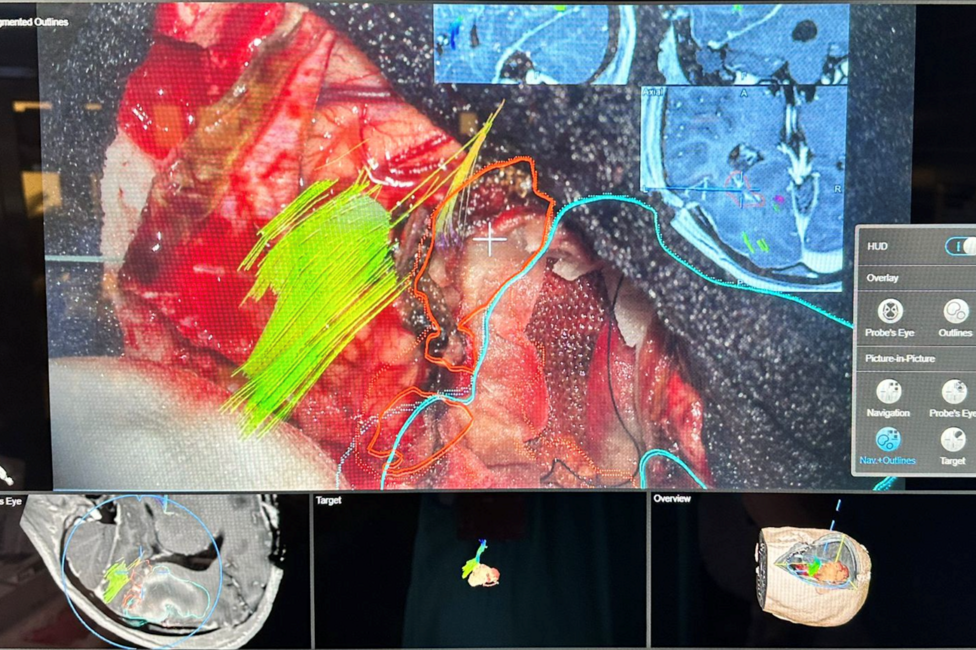
An operating microscope functioning as a “head-up display” (HUD), an MRI scanner located directly next to the operating table, and a navigation system that guides surgeons through the brain with millimeter precision—what sounds like science fiction is everyday clinical practice at the Medical University of Vienna. Univ.-Prof. Karl Rössler and his team have tested these technologies in large patient cohorts and demonstrated that improved orientation often enables more extensive resections—resulting in better outcomes while maintaining a high level of safety.
Why Brain Navigation Is Such a Complex Task
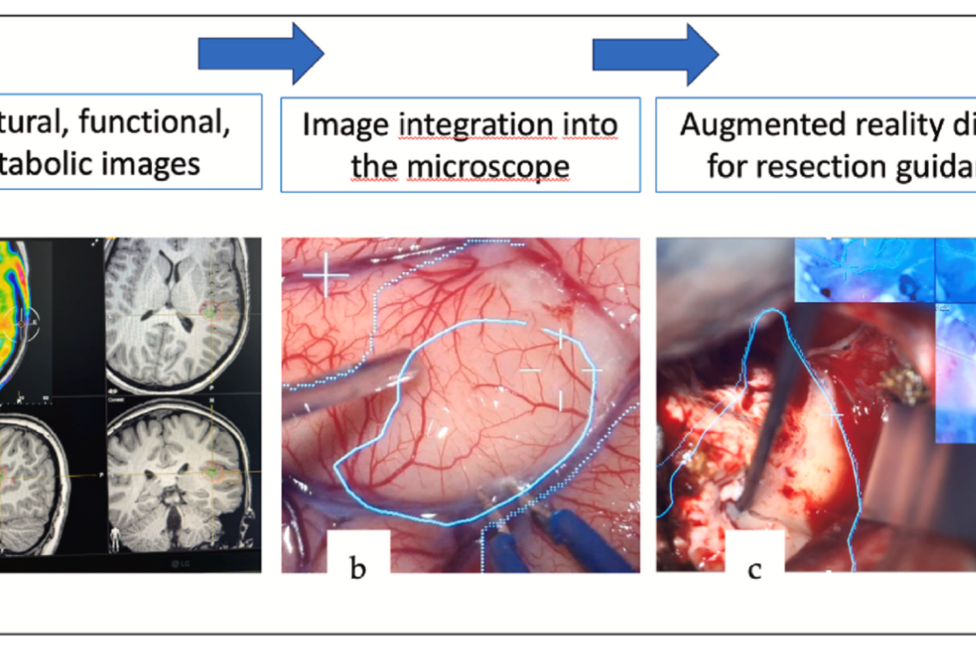
During surgery, the brain shifts (“brain shift”). In addition, critical functional areas—such as language, motor, and visual cortex—are often located in close proximity to tumors or epileptogenic foci. Preoperative planning alone is therefore insufficient; the surgical team requires “live data” during the operation and a visualization that remains within the surgeon’s field of view. This is exactly where neuronavigation, intraoperative MRI (iMRI), and augmented reality (AR) work together.
Intraoperative MRI: A Second Pair of Eyes in the Operating Room
The team led by Rössler has used intraoperative MRI (iMRI) in hundreds of epilepsy surgeries. The result: more frequent complete resections and improved seizure freedom, without an increase in complication rates. In a large series of 415 cases, Engel class I outcomes (seizure freedom) were significantly more common; iMRI revealed residual lesions and often prompted a “second look” during the same anesthesia.
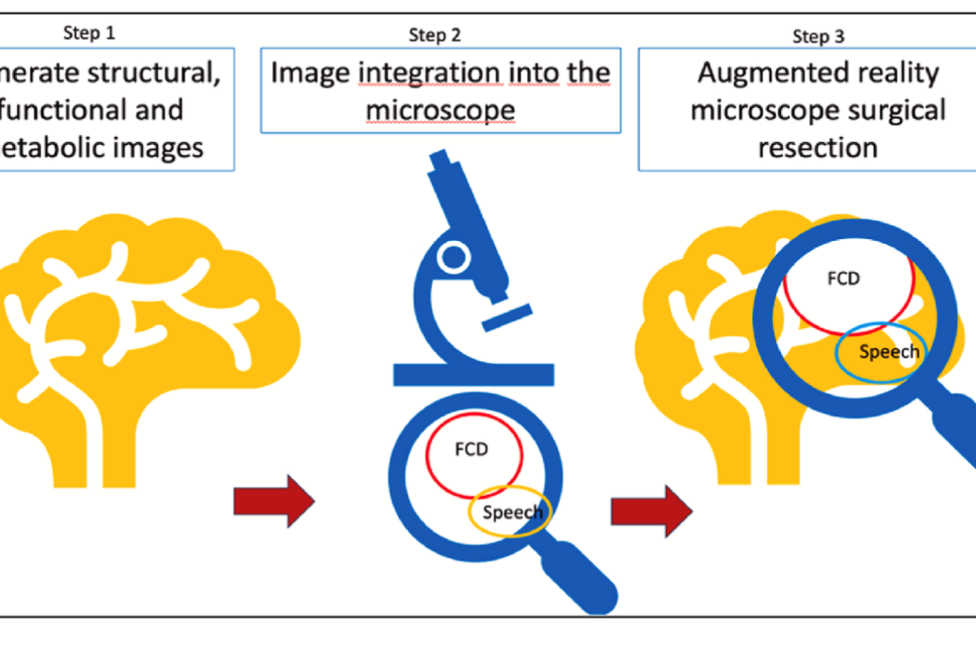
In patients with focal cortical dysplasia (FCD) type II—a developmental brain disorder associated with epilepsy—iMRI in combination with neuronavigation also resulted in significantly better seizure outcomes, particularly when an additional intraoperative resection was required.
Focus on Pediatric Epilepsy Surgery
Since 2020, a 3-tesla two-room iMRI concept has been in operation at the Department of Neurosurgery of the Medical University of Vienna. In 148 procedures performed in 124 children, iMRI optimized surgical outcomes in approximately one quarter of cases, while maintaining high safety standards—without additional infection- or positioning-related complications.
Conclusion: iMRI is not required in every case, but it is crucial in selected situations. A meta-analysis conducted by the Vienna team reinforces this conclusion, showing that iMRI improves extent of resection and seizure control in epilepsy surgery.
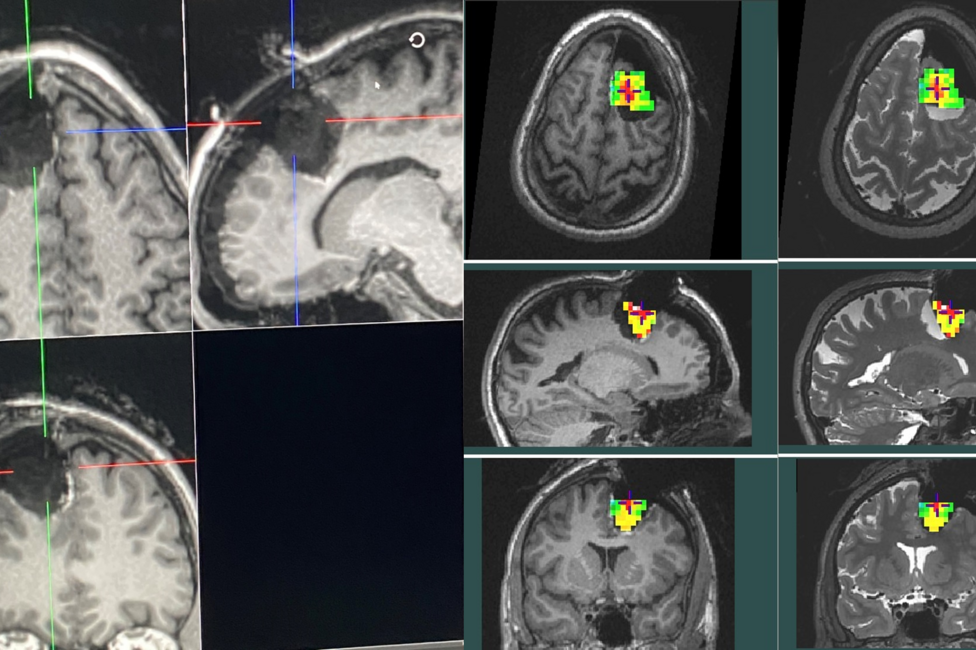
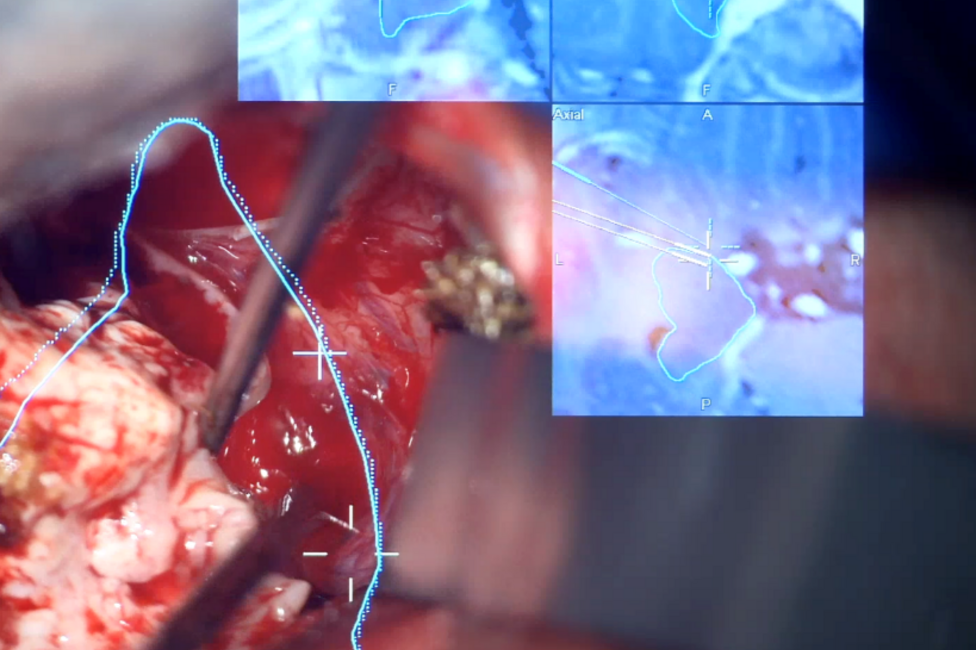
AR & HUD in the Microscope: Data in the Surgeon’s Line of Sight
While iMRI provides “new” images during surgery, AR brings existing information—such as segmentations of tumors, vessels, and fiber tracts—directly into the eyepiece of the operating microscope. The head-up display overlays virtual contours onto the real surgical field, eliminating the need to shift the gaze to separate monitors. Studies on microscope-based AR demonstrate high registration accuracy, improved orientation, and rapid intraoperative accuracy checks. In skull base surgery and transsphenoidal procedures, AR helps protect critical structures.
How the Trio Works Together
- Neuronavigation links preoperative imaging (MRI/fMRI/DTI) with the patient’s anatomy during surgery.
-
AR head-up display (HUD) makes these navigation data visible as overlays—in real time, through the microscope.
-
iMRI updates the entire navigation setup as needed and verifies whether the surgical target has been reached.
Especially for lesions near eloquent areas (language/motor cortex) in tumor and epilepsy surgeries, this combination enables maximal resection with minimal risk.
Benefits for Patients
-
Higher chance of complete tumor or lesion removal.
-
Improved seizure control in epilepsy surgery (often Engel class I).
-
Increased safety: iMRI immediately detects residual tissue; AR/HUD reduces orientation errors.
Medical University of Vienna – Profile and Expertise
Since taking the helm of the Department of Neurosurgery in 2019, Karl Rössler has been driving the advancement of AI-driven and image-guided, navigated neurosurgery at the Medical University of Vienna. This effort is carried out in an interdisciplinary context with neurology, pediatrics, and neuroradiology within the Comprehensive Center for Clinical Neuroscience and Mental Health (C3N-MH), bringing the Department of Neurosurgery into the international spotlight.