Neurosurgery of the Future: Electronics and Digitization in Medical Technology
The process of digitalization is also in full swing in neurosurgery and is revolutionizing the surgical techniques and landscapes. Our surgeons and scientists are committed participants in this process.
Combining structural, functional and metabolic image data to create a procedure-specific multimodal image
Neuronavigation systems have a long tradition at the University Department of Neurosurgery in Vienna, and today navigation systems are used in almost all areas of neurosurgery.
The Neuronavigation Working Group is continuously developing and publishing specialized image fusion protocols for glioma, skull base and pituitary surgery.
The fiber tract architecture of the brain was illustrated in a unique combination of anatomical dissection and electronic imaging, providing multimodal image fusion concepts especially for Glioma Surgery.
The existing multimodal fusion protocol for Transnasal Pituitary Surgery was extended to include a special CT surface representation of the endonasal anatomy, which has made it possible to clearly identify the finest structures (e.g. thin septations). MR angiographic imaging has also been improved to specifically identify fine vessels (e.g. sphenopalatine artery). This protocol is intended to enhance the safety of endoscopic transsphenoidal procedures.
For Skull Base Surgery, a special navigation protocol was developed using the example of sphenoorbital meningiomas in order to remove soft tumour parts as well as tumor-altered bones to the fullest extent possible while protecting neurovascular structures.
In 2019, two additional BrainLab navigation systems became available, complementing the existing pair of Medtronic navigation systems.
The simulator is used to complete surgical training and plan operations in a realistic anatomical environment
For preoperative intervention planning, four Workstations are available in our clinic, on which a 3D simulation of the individual patient anatomy is possible.
A 3D Haptic Simulator, developed in cooperation with the National Research Council Canada, is used as part of neurosurgical training and ongoing scientific projects, thus enabling learning and practicing microsurgical skills in a 3D neurosurgical imaging environment. The user receives haptic feedback on the surgical instruments and a score to evaluate their own performance.
For training and teaching, facilities for the three-dimensional visualization of anatomy are now also available at the microsurgical laboratory. In addition to a surgical microscope with a 3D video recording option, a robotic photo camera has been developed that enables the automated acquisition of 3D images.
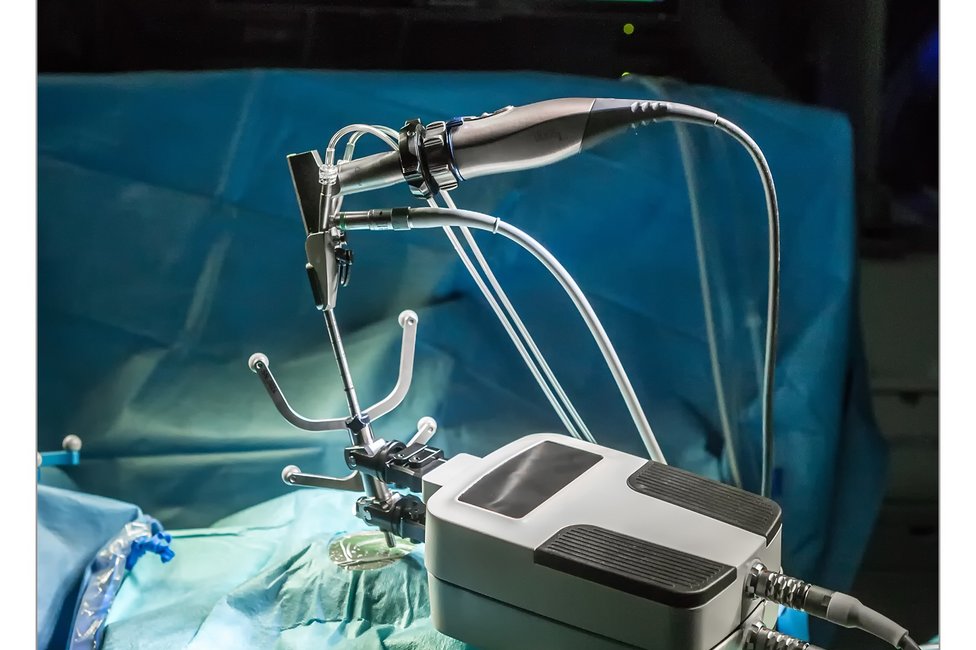
Robot-assisted neurosurgery
Since 2012, the Department of Neurosurgery has been using a miniaturized robotic system developed in Austria for stereotactic interventions (e.g. biopsies, deep electrode implantations) as part of a feasibility and development study. This robotic system is the first device to combine the advantages of high positioning accuracy (≤ 0.1mm) while taking into account the limited space available in the operating theatre. It was shown that the robot does not influence operating theatre routines thanks to its miniaturised design and compatibility with the existing navigation system, meaning that it does not prolong the duration of the operation either.
The prototype of the robotic system was tested in multicentre trials (Vienna, London, Milan) and further developed at our clinic. An instrument and drilling system was implemented that allows more precise and minimally invasive biopsies compared to conventional procedures.
As of 2019, the robot has been approved for stereotactic biopsies, implantation of depth electrodes for stereoEEG and laser ablation.
Roboter-navigierte Laser-Kraniotomie für die Implantation von Tiefenelektroden in der Epilepsie-Chirurgie
In recent years, we have been working closely with Advanced Osteotomy Tools, a Swiss MedTech company, to expand the indications for a laser which has already been certified in oral and maxillofacial surgery to include neurosurgical operations.
The specific goal of the peer-reviewed studies published so far was to optimize the implantation of depth electrodes in epilepsy surgery. The frameless stereotactic method with robotic guided laser ablation was tested for the first time in a cadaver (Roessler et al., Journal of Neurological Surgery 2020 Robotic Navigated Laser Craniotomy for Depth Electrode Implantation in Epilepsy Surgery: A cadaver lab study).
Here, target point accuracies of 2.0 mm (+/- 0.64SD) were achieved for frontal, parietal, and occipital depth electrode trajectories planned using preoperative CT datasets. Implantation time was 10-15 minutes per electrode, with laser ablation taking just under one minute.
These results were subsequently confirmed in several in-vivo non-recovery studies in pigs: (Winter et al., Frontiers in Robotics and AI. 2021: Navigated, Robot-Driven Laser Craniotomy for SEEG Application Using Optical Coherence Tomography in an Animal Model).
It should also be mentioned here that no anesthesiological problems occurred during the operations and the animals all survived the laser ablations. The results of the first in vivo recovery study, which was performed on sheep at MedUni Vienna, still require further analysis and evaluation before the first pilot studies can be conducted on humans.
The conclusion so far is that navigated robot-assisted laser craniotomies for deep electrode implantation may be a promising new alternative to conventional frameless hand-guided craniotomies.
Team of the Navigation, Simulation and Robotics Working Group
Head
Assoc. Prof. Priv.-Doz. Dr.med.univ. Christian Dorfer
E-Mail: christian.dorfer@meduniwien.ac.at
Univ.-Prof. Dr.med.univ. Karl Rössler
E-Mail: karl.roessler@meduniwien.ac.at
Deputy:
Dr. med.univ. Fabian Winter
E-Mail: fabian.winter@meduniwien.ac.at